MPOX
(Formerly known as Monkeypox)What is mpox?
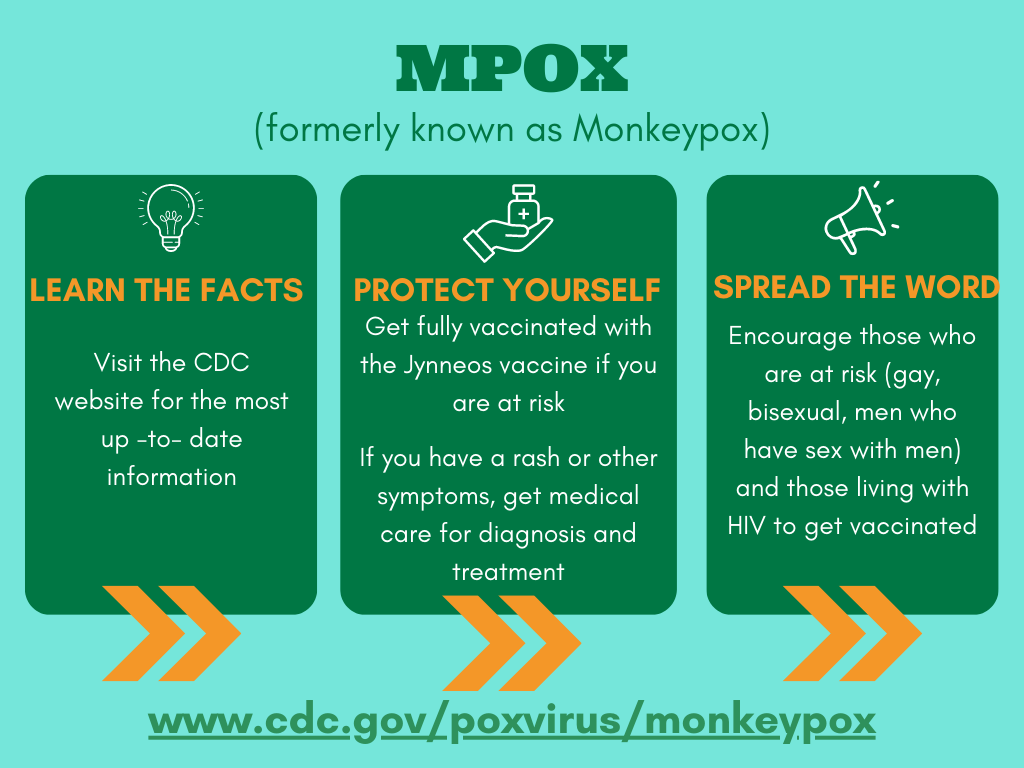
Mpox, formerly known as monkeypox, is an orthopox virus formerly found mostly in Africa. In May of 2022 a world-wide outbreak occurred mostly in gay, bisexual and other men who have sex with men. The outbreak peaked in early August of 2022 at about 450 new cases daily. For current data, visit CDC website
Although most infections seem to be associated with sexual activity, transmission may occur from other skin to skin contact with infected persons or through sharing of objects and materials that someone with mpox has used. Women and children have been infected – consequently all persons exposed to a person with mpox have some risk.
As of February 2023 there are about 3 new cases daily in the US. The reasons for the decline in cases are not fully understood but education, risk behavior change, available antiviral therapy and vaccination are all felt to contribute.
The CDC has extensive information for individuals and for healthcare professionals. These sites are updated regularly.
Information for Individuals:
https://www.cdc.gov/poxvirus/monkeypox/your-health/index.html
Information for Healthcare Providers:
https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.html
If you have been exposed:
If you know you have been exposed to someone with mpox, vaccination with Jynneos within a few days of exposure may prevent or decrease the severity of illness.
Mpox Symptoms
People with mpox often get a rash that may be located on hands, feet, chest, face, or mouth or near the genitals, including penis, testicles, labia, and vagina, and anus. The incubation period is 3-17 days. During this time, a person does not have symptoms and may feel fine.
- The rash will go through several stages, including scabs, before healing.
- The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of mpox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g., sore throat, nasal congestion, or cough)
You may experience all or only a few symptoms
- Sometimes, people have flu-like symptoms before the rash.
- Some people get a rash first, followed by other symptoms.
- Others only experience a rash.
If you have symptoms:
Avoid contact with others and do not share household items.
Seek medical care right away for diagnosis and possible treatment.
Mpox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
A person with mpox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. Some people have been found to have infection but no symptoms.
Most persons with Mpox will recover without treatment but some groups are at higher risk for severe disease.
These groups include:
- People currently experiencing severe immunocompromise due to conditions such as advanced or poorly controlled human immunodeficiency virus (HIV), leukemia, lymphoma, generalized malignancy, solid organ transplantation, therapy with alkylating agents, antimetabolites, radiation, tumor necrosis factor inhibitors, high-dose corticosteroids, being a recipient of a hematopoietic stem cell transplant <24 months post-transplant or ≥24 months but with graft-versus-host disease or disease relapse, or having autoimmune disease with immunodeficiency as a clinical component1
- Pediatric populations, particularly patients younger than 1 year of age
- Pregnant or breastfeeding people2
- People with a condition affecting skin integrity — conditions such as atopic dermatitis, eczema, burns, impetigo, varicella zoster virus infection, herpes simplex virus infection, severe acne, severe diaper dermatitis with extensive areas of denuded skin, psoriasis, or Darier disease (keratosis follicularis)
Treatment is available with antiviral drugs including tecovirimat (TPOXX).
Treatment should be considered for use in people who have the following clinical manifestations:
- Severe disease — consider severe disease when a patient has conditions such as hemorrhagic disease; a large number of lesions such that they are confluent; necrotic lesions; severe lymphadenopathy that can be necrotizing or obstructing (such as in airways); involvement of multiple organ systems and associated comorbidities (for example, pulmonary involvement with nodular lesions; sepsis; encephalitis; myocarditis; ocular or periorbital infections); or other conditions requiring hospitalization
- Involvement of anatomic areas which might result in serious sequelae that include scarring or strictures — these include lesions directly involving the pharynx causing dysphagia, inability to control secretions, or need for parenteral feeding; penile foreskin, vulva, vagina, urethra, or anorectum with the potential for causing strictures or requiring catheterization; anorectal lesions interfering with bowel movements (for example, severe pain); and severe infections (including secondary bacterial skin infections), especially those that require surgical intervention such as debridement.
Treatment should also be considered for use in people who are at high risk for severe disease (as noted above). For patients at high risk for progression to severe disease, treatment should be administered early in the course of illness along with supportive care and pain control.
Protect Yourself:
- Avoid close skin to skin contact with people who have a rash that looks like mpox.
- Avoid contact with objects and materials that a person with mpox has used.
- Wash your hands often.
- Get vaccinated with the Jynneos vaccine. Remember: two vaccine doses 4 weeks apart are needed for maximum protection.
Vaccine Information: https://www.cdc.gov/poxvirus/monkeypox/vaccines/index.html
Mpox and HIV:
Current data suggest that about 40% of people diagnosed with mpox in the United States also had HIV (human immunodeficiency virus). CDC is still learning if having HIV increases the likelihood of getting sick with mpox if exposed to the virus. However, we do know that people with severe immunocompromise (like advanced HIV) are at increased risk of severe mpox, or even death, if they become infected.
CDC recommends vaccination for people who have been exposed to mpox virus and people who may be more likely to get mpox. There are currently two vaccines (JYNNEOS and ACAM2000) that can be used to prevent mpox.
- JYNNEOS vaccine is authorized for the prevention of mpox and is considered safe for people with HIV. This is the vaccine currently being offered in the United States.
Safer Sex and Social Gatherings:
Vaccination is an important tool in preventing the spread of mpox (formerly known as monkeypox). If you are at risk for mpox but haven’t received your two-dose vaccine yet, temporarily changing some parts of your sex life might reduce the risk of exposure to the virus. This includes the time between your first and second shots of vaccine. Your protection will be highest two weeks after your second dose of vaccine.
Make a habit of exchanging contact information with any new partner to allow for sexual health follow-up, if needed.
Talk with your partner about any mpox symptoms and be aware of any new or unexplained rash or lesion on either of your bodies, including the mouth, genitals (penis, testicles, vulva, or vagina), or anus (butthole). If you or your partner has or recently had mpox symptoms, or you have a new or unexplained rash anywhere on your body, do not have sex and see a healthcare provider. In some cases, symptoms may be mild, and some people may not even know they have mpox.
If you or a partner has mpox or think you may have mpox, the best way to protect yourself and others is to avoid sex of any kind (oral, anal, vaginal) and kissing or touching each other’s bodies—while you are sick. Especially avoid touching any rash. Do not share things like towels, fetish gear, sex toys, and toothbrushes.
Even if you feel well, here are some ways to reduce your chances of being exposed to mpox if you are sexually active:
- Take a temporary break from activities that increase exposure to mpox until you are two weeks after your second dose. This will greatly reduce your risk.
- Limit your number of sex partners to reduce your likelihood of exposure.
- Spaces like back rooms, saunas, sex clubs, or private and public sex parties, where intimate, often anonymous sexual contact with multiple partners occurs—are more likely to spread mpox.
- Condoms (latex or polyurethane) may protect your anus (butthole), mouth, penis, or vagina from exposure to mpox. However, condoms alone may not prevent all exposures to mpox since the rash can occur on other parts of the body.
- Gloves (latex, polyurethane, or nitrile) might also reduce the possibility of exposure if inserting fingers or hands into the vagina or the anus. The gloves must cover all exposed skin and be removed carefully to avoid touching the outer surface.
- Avoid kissing or exchanging spit since mpox can spread this way.
- Masturbate together at a distance without touching each other and without touching any rash.
- Have virtual sex with no in-person contact.
- Consider having sex with your clothes on or covering areas where rash is present, reducing as much skin-to-skin contact as possible. Leather or latex gear also provides a barrier to skin-to-skin contact; just be sure to change or clean clothes/gear between partners and after use.
- Be aware that mpox can also spread through respiratory secretions with close, face-to-face contact.
- Remember to wash your hands, fetish gear, sex toys, and any fabrics (bedding, towels, clothes) after having sex.